LI-RADS Value As A Prognostic Tool In Patients At High Risk For Liver Cancer
LR-M category and nontargetoid features were negatively associated with survival independent of histopathologic characteristics

The Liver Imaging Reporting and Data System (LI-RADS) is an established standardized interpretation and reporting system that is specific for the imaging diagnosis of hepatocellular carcinoma (HCC) in high-risk patients.
“LI-RADS was developed as a means of achieving reliable classification without the need for biopsy in patients with cirrhosis, chronic hepatitis B, a history of HCC or current HCC,” explained Maxime Ronot, MD, PhD, a radiologist at the Beaujon University Hospital in Clichy, France and member of the American College of Radiology LI-RADS steering committee.
LI-RADS utilized imaging features seen on CT, MRI, or contrast-enhanced ultrasound (CEUS) to assign hierarchical categories that communicate the likelihood of HCC, with LR-1 being definitely benign and LR-5 as definitely HCC. Observations assigned to the LR-M category are most likely malignant but not specifically HCC, although approximately one-third of observations listed as LR-M correspond to HCC.
While LI-RADS has gained momentum for the non-invasive diagnosis of liver cancer, especially in western countries, could it also be used as a prognostic tool in patients at high risk for HCC?
That’s the question posed by a Radiology study co-authored by Dr. Ronot.
“The prognostic value of pathology is well known. We wanted to see whether or not the LI-RADS system could also be used to predict the likelihood of recurrence of cancer after surgery,” Dr. Ronot said.
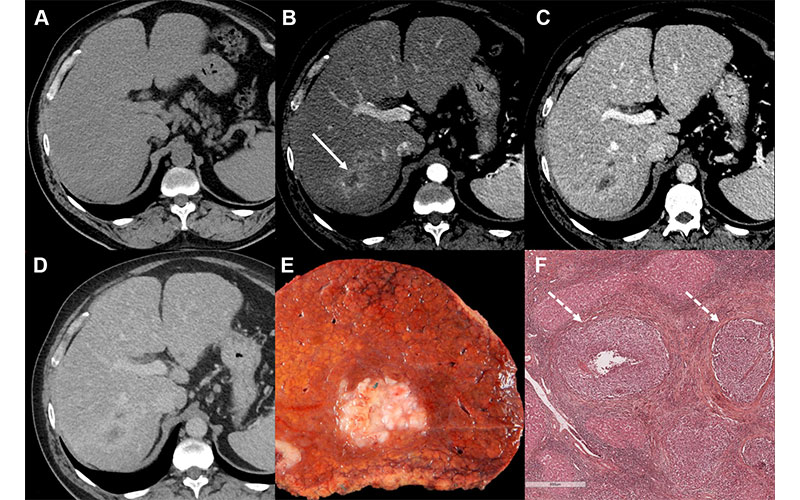
Images in a 55-year-old male patient with a history of hepatitis C virus–related cirrhosis and a 45-mm hepatocellular carcinoma (HCC). Axial (A) precontrast and (B–D) contrast-enhanced CT images in the (B) hepatic arterial, (C) portal venous, and (D) delayed phases show lesion (arrow in B) with rim arterial phase hyperenhancement categorized as Liver Imaging Reporting and Data System category LR-M. (E) Photograph of resected specimen shows a poorly demarcated HCC. (F) Photomicrograph (hematoxylin-eosin stain) reveals a poorly differentiated HCC with microvascular invasion (arrows). Scale bar in F = 600 µm. Intrahepatic recurrence was observed at 14 months after resection. https://doi.org/10.1148/radiol.231160 ©RSNA 2024
The Prognostic Value of All Imaging Features
The study analyzed a group of patients with liver cancer who underwent surgery.
“The study leveraged the fact that our department benefits from excellent collaboration with our pathology colleagues and that our hospital has a very high volume of patients with liver cancer and HCC,” Dr. Ronot said.
Having collected all pertinent medical information about the patients—including liver disease and tumor characteristics—researchers described the tumor imaging features using the LI-RADS features, terminology and categories.
Next, researchers studied the patient outcomes, looking at whether there was a recurrence of the disease or if a patient died because of the cancer. They also looked at all the details of the pathological reports and analyzed if the imaging features were independently associated with a recurrence, even when considering pathology.
Based on this work, the study confirmed that some imaging features used for diagnosing HCC are indicators of a higher risk of recurrence.
Take, for instance, the LR-M categorization.
According to Dr. Ronot, an LR-M categorization is often assigned to tumors with a targetoid appearance.
“When you see that feature, you can directly classify the tumor as LR-M, which indicates it as being more aggressive and thus more likely to recur,” he said.
Aside from the obvious targetoid appearance, many other, perhaps less obvious, LR-M features may also appear in an image.
“The fact that the tumor is infiltrative, that you can see necrosis or marked diffusion restriction in the tumor, is not enough to categorize the tumor as LR-M,” Dr. Ronot said. “But it doesn’t mean these features aren’t useful.”
However, because they aren’t sufficient to classify a tumor as LR-M, or because the radiologist already knows it’s a cancer, these features tend to be completely disregarded.
According to Dr. Ronot, that’s a mistake.
“Our study shows that regardless of LI-RADS category, these features have an important prognostic value,” he said.
To illustrate, Dr. Ronot points to a tumor categorized as LR-5, the highest probability for hepatocellular carcinoma.
“Typically, once such a categorization is made, the radiologist’s work stops,” Dr. Ronot explained. “We want to take this one step further and, in addition to the LR-5 categorization, encourage radiologists to note whether the tumor also displays features of aggressiveness that could further inform discussions on how to treat or manage the disease.”
Paying Attention to Tumor Appearance
But therein lies the challenge: ensuring that these additional features are integrated into the treatment decision-making process.
Usually, the decision to choose a treatment is based on patient history and health status, the quality of the liver and simple tumor characteristics like size and number, according to Dr. Ronot. “However, this research suggests that the behavior of the tumor might correspond also to an additional group of factors that should be given attention when deciding which treatment is better.
“By expanding the uses of LI-RADS and refining its role as a prognostic tool, we can pave the way for radiologic information to have an even greater impact on patient management and wellbeing,” Dr. Ronot concluded.
For More Information
Access the Radiology study, “Association of LI-RADS and Histopathologic Features with Survival in Patients with Solitary Resected Hepatocellular Carcinoma.”
Read previous RSNA News stories about LI-RADS: