Molecular Markers Star in Latest Guidance for Head and Neck Tumors
What the radiologist should know

In concert with the RadioGraphics monograph, RSNA News shares the latest in head and neck imaging.
Genomics has revolutionized tumor taxonomy and classification, and rapid advances in molecular imaging place radiologists at the helm.
The 5th edition of WHO Classification of Head and Neck Tumors, published in full this year, includes major updates based on tumors’ distinctive molecular and genetic characteristics. And for the first time, a radiologist serves on the World Health Organization’s Head and Neck editorial board.
“There is strong interest in finding the imaging correlates of the newly recognized tumor entities,” said Amit Agarwal, MBBS, MD, from the Mayo Clinic in Jacksonville, FL. “Radiologists are playing a vital role in the multidisciplinary team for tumor management.”
In a recent paper published in RadioGraphics, Dr. Agarwal and colleagues detailed the genetic and molecular markers that will quickly become essential to diagnosis, management and staging.
The Concepts Radiologists Should Know
With the advent of guidance based on molecular markers and genetics—and an increased emphasis on imaging—the authors provided an overview of concepts.
The authors review preferred techniques, gold standards and emerging applications in hematoxylin and eosin staining, immunohistochemistry, and genetic evaluation, highlighting the molecular characteristics of epithelial and non-epithelial tumors of the head and neck.
Among the newer techniques described is “liquid biopsy,” which is used to detect circulating tumor cells and DNA from blood samples. It’s currently FDA approved for lung and breast carcinomas.
Dr. Agarwal also noted that there are new prognostic and predictive markers that will make it easier to identify tumors.
“In the context of worldwide access to certain testing modalities—such as immunohistochemistry and genetic studies—the tumors are, for the most part, still defined by their histological features, utilizing ancillary testing to narrow the diagnosis when required,” explained Dr. Agarwal. “However, with a continued decrease in cost and wider availability, we expect these tests to become more common in different parts of the world.”
For epithelial tumors, two molecular markers of interest are p16 for HPV-induced oropharyngeal squamous cell carcinomas and EBV-encoded small RNAs for EBV-related nasopharyngeal carcinomas. The authors cover diagnostic and prognostic guidance for a range of squamous cell carcinomas and discuss what radiologists can expect to encounter in the molecular imaging realm.
New markers in non-squamous cell tumors appear in the 5th edition WHO guidelines for muscle, neural, vascular and epithelial differentiation.
“Another prominent change is that tumor types common to multiple systems are clubbed together with separate chapters on mesenchymal, melanocytic, hematolymphoid, and neuroendocrine tumors,” the authors explained. “For the first time, WHO introduced a chapter on genetic tumor syndromes, given the increasing importance of genetics in tumor biology and behavior over the past decade and the identification of germline mutations in a higher number of apparent ‘sporadic’ diseases.”
Classification guidance for salivary and sinonasal neoplasms has undergone the most significant overhaul, moving to different categories—and in some cases redefined as separate entities—thanks to molecular markers. In addition, “there are numerous other updates to the tumor types common to multiple systems that are dealt with together, like those on mesenchymal, melanocytic and hematolymphoid tumors,” the authors said.
WHO has dedicated a new section to reflect increased focus on the diagnostic molecular pathologies of tumor-associated syndromes, which are now part of WHO’s “essential” criteria for diagnosis.
“All the genetic syndromes have now been defined by their molecular and genetic signature, with personalized treatment and follow-up recommendations for patients,” the authors said. “Knowledge about these syndromes has enabled the identification of at-risk individuals in affected families, who can then be offered genetic counseling.”
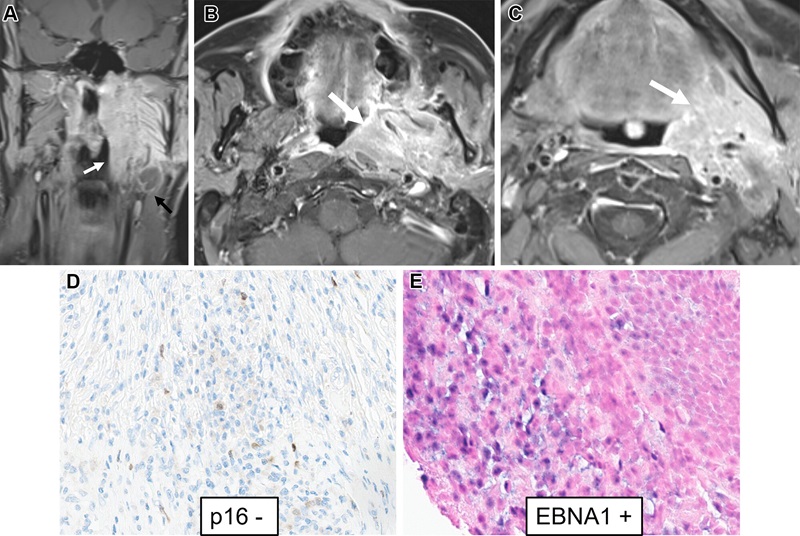
EBV-induced nasopharyngeal carcinoma in a 55-year-old man. (A–C) Coronal (A) and axial (B, C) contrast-enhanced fat-suppressed T1-weighted MR images show a large infiltrative mass involving the nasopharynx and oropharynx, extending from the skull base to the base of the tongue (white arrow). Definite localization of the primary site (nasopharyngeal vs oropharyngeal) was not clear at clinical and radiologic evaluation. Fine-needle aspiration of the metastatic left submandibular lymph node (black arrow in A) was performed. (D, E) Photomicrographs with IHC stain show negative staining for p16 (D) and positive staining for EBV nuclear antigen (EBNA1) (E) in the tumor cells. EBV BamHI-W DNA was detected with a blood test (liquid biopsy), and ISH showed abundant EBV-encoded small RNAs, confirming the diagnosis of nasopharyngeal carcinoma. https://doi.org/10.1148/rg.240037 © RSNA 2024
Staying Abreast of “A Flood of Information”
Major advances in the way clinicians understand cancer biology will lead to specific treatment paradigms for a wide range of head and neck neoplasms, and radiologists must be ready, Dr. Agarwal advised.
In the next few years, he commented, radiologists can expect to see quicker scans with higher sensitivities as deep-learning sequences begin to integrate into clinical practice. The specialty will see dedicated protocols—especially in MRI—that will provide a more personalized approach to diagnosis.
“This new understanding will pave the way for targeted treatment strategies as the next step in precision medicine,” Dr. Agarwal said. “Radiologists must be familiar with these changes as we integrate this information into our clinical practice, and as a key member of the multidisciplinary team.”
For More Information
Access the RadioGraphics article, “Molecular Markers of Head and Neck Tumors.”
Read previous RSNA News stories on head and neck imaging: