Imaging Pulsatile Tinnitus: A State-of-the-Art Review
Common complaint can be severely debilitating and imaging can help guide treatment

In concert with the RadioGraphics monograph, RSNA News shares the latest in head and neck imaging.
Radiologists must take a closer look at the clinical context and develop more familiarity with subtle imaging clues in patients with pulsatile tinnitus. Building expertise in identifying findings that often go unseen can aid in decision-making and improve patient care.
“Tinnitus is such a common problem that 70% of us will experience it at some point in our lives,” said Suyash Mohan, MD, associate professor of radiology and director of neuroradiology research at the University of Pennsylvania (UPenn) in Philadelphia. “Sometimes it may be transient and harmless and other times it can greatly affect quality of life and be quite problematic.”
Dr. Mohan coauthored a RadioGraphics review that provides a systematic, targeted approach based on physical examination findings and includes novel management strategies.
“So much of radiology is knowing where to look, which is particularly relevant in the setting of pulsatile tinnitus. Education and training are important, and if you don’t know where to look, you will almost always miss the subtle findings,” Dr. Mohan said.
“Tinnitus is such a common problem that 70% of us will experience it at some point in our lives. Sometimes it may be transient and harmless and other times it can greatly affect quality of life and be quite problematic.”
—SUYASH MOHAN, MD
Investigating Clinical Context, Identifying Imaging Clues
Defined as the perception of a heartbeat sound without external stimulus, pulsatile tinnitus is often caused by disorders or malformations in the blood vessels or arteries—especially those near the ears—that can change blood flow through the affected blood vessels.
Although it is less common than non-pulsatile tinnitus, Dr. Mohan said pulsatile tinnitus may point to an underlying pathologic condition with potentially devastating effects.
“We created this state-of-the-art review to help in understanding the nuances associated with pulsatile tinnitus, provide diagnostic pathways and point out commonly missed subtleties,” Dr. Mohan said. “This condition has a variety of causes—some of which are life threatening. It not only causes anxiety in patients, it also causes anxiety in the physician evaluating these patients because the imaging looks bland, and the findings are subtle.”
For patients with tinnitus, evaluation begins with a careful history and physical examination. In the case of pulsatile tinnitus, the examination should include auscultation of the neck, ear and surrounding structures.
Clues such as the pitch of the tinnitus, changes in the sound based on head or body position, the presence of hypercoagulability, bony structural causes or middle-ear masses may point to venous and arterial causes or other etiologies that can help guide the radiologist.
“Any cause of conducive hearing loss, such as fluid in the middle ear, can lead to pulsatile tinnitus, but for patients with the absence of hearing loss, the initial workup should include an MRA/MRV or CTA/CTV to look for arterial or venous causes,” said review coauthor Suehyb G. Alkhatib, MS, MD, a neurointerventional radiologist at Radiology Associates of Richmond in Virginia who maintains a joint affiliation with UPenn. “If you’re attuned to the clinical history, you know which side the tinnitus is on and you know the nature of the tinnitus, you can start to hone-in on finer imaging details in the cases we present in our review article.”
Self-described as a “less-is-more” physician, Dr. Alkhatib said his perspective is changing. “There are over 50 images in the paper reflecting 20 patients. About half of those who underwent treatment had findings that were not noted on their initial imaging studies. Had the subtle findings been identified, we may have avoided unnecessary additional imaging,” he said.
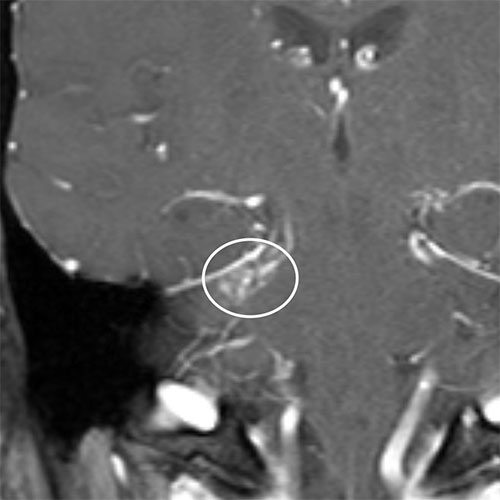
Asymmetric enhancement was questioned on a coronal T1W contrast enhanced MRI in a 34-year-old man with right sided pulsatile tinnitus. The patient underwent catheter angiography which confirmed a small right cerebellar arteriovenous malformation treated with stereotactic radiosurgery (SRS).
https://doi.org/10.1148/rg.240030 © RSNA 2024
Embracing Evolving Tools and Techniques
“The imaging and management of pulsatile tinnitus are rapidly evolving,” Dr. Alkhatib said. “There are things we are doing nowadays that were rare five years ago.”
Diagnostic imaging approaches for the condition depend on a patient’s clinical presentation and the suspected disease origin. Dr. Alkhatib said emerging diagnostic imaging options include four-dimensional CT or multiphase MRI/MRA, which may offer temporal resolution of contrast physiology without the inherent risks that come with catheter angiography.
“These approaches have risks such as radiation with CT and longer imaging time on MRI, which may present a resource challenge,” Dr. Alkhatib said.
He acknowledged that both methods require more imaging, which can increase the mental burden on the radiologist interpreting the image. “Sometimes though, these methods can be the difference between finding and missing some of the more subtle abnormalities that cause pulsatile tinnitus.”
Interest in the treatment of pulsatile tinnitus is increasing across the neurointerventional world, according to Dr. Alkhatib who noted that newer approaches are gaining traction. “It was rare to stent five or ten years ago, and the thought was that a lot of these findings did not cause symptoms. Early on, some questioned why we were stenting,” he said. “However, anecdotally, we know that a greater proportion of those we treat improved. Now we are trying to assess which patient population will benefit from stenting. It’s more than we thought five or ten years ago.”
Drs. Alkhatib and Mohan and colleagues are working to identify characteristics that might predict the lack of treatment response to exclude patients when appropriate and avoid associated risks. They emphasize the power of knowledge in finding a cure for patients with pulsatile tinnitus.
“Our review paper is full of practical and useful teaching points,” Dr. Mohan said. “Readers will find a structured framework that aids not just radiologists but also ENT surgeons, neurosurgeons, endovascular specialists and other clinicians in identifying an underlying diagnosis and formulating a management plan for these patients.”
For More Information
Access the RadioGraphics article, “Imaging of Pulsatile Tinnitus.”
Read previous RSNA News stories on head and neck imaging: