Dual-Energy CT and Cinematic Rendering Can Take Guesswork Out of Pelvic Fracture Grading
New method can provide comprehensive evaluation of images while keeping patients stabilized

For trauma patients presenting with pelvic ring disruptions, dual-energy CT and cinematic rendering can illuminate fracture patterns that might be cloaked by anatomic reduction from pelvic binders.
Pelvic binders, or provisional circumferential compression devices, are often used to help control hemorrhage in trauma patients who present with pelvic ring disruptions, but the reduction they induce can mask the severity of the injury on conventional single-energy or single-energy equivalent CT, said Theresa Yu, MD, of the University of Maryland and R. Adams Cowley Shock Trauma Center.
“Binder off” CT or plain radiographic imaging is risky because of the threat of releasing tamponade and allowing sharp bone ends to shift.
Dr. Yu’s team explored a method that might provide a more comprehensive evaluation of images while keeping vulnerable patients stabilized.
“We found that radiologists were better able to diagnose and grade pelvic fracture instability in these patients when conventional single-energy equivalent CT images— reflecting the current imaging standard—were used in combination with dual-energy CT and cinematic rendering,” she said.
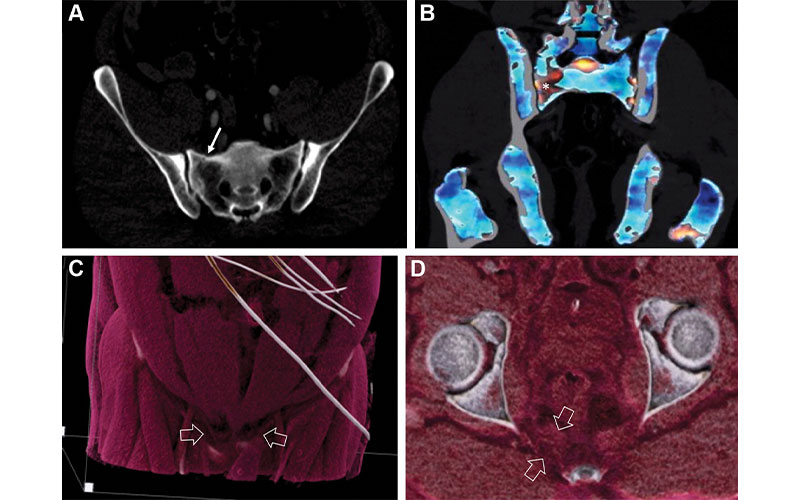
Images in a 42-year-old male pedestrian struck by a moving vehicle.
Yu et al, Radiology 2022; https://doi.org/10.1148/radiol.211679 ©RSNA 2022
Identifying Instability In Patients With Pelvic Binders
In a novel study published in Radiology, Dr. Yu and her colleagues demonstrated that pairing these modalities enabled radiologists to confidently grade the severity of pelvic instability.
“The pelvis is a special case because you are often dealing not only with mechanical instability—requiring provisional stabilization and then open or percutaneous fixation with combinations of plates and screws—but also with vascular injuries that are potentially lethal,” said David Dreizin, MD, last author on the study and associate professor, diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore. “The degree of pelvic instability is an important indirect marker of bleeding risk.”
Hemorrhage may not present as “textbook” contrast extravasation on the admission study for a variety of reasons, including transient vessel occlusion, spasm, tamponade, or factors related to scan timing, he explained.
Particularly exciting is the “MRI-like” visualization the combined techniques can provide with respect to osteoligamentous integrity, Dr. Dreizin said.
Dual-energy CT provides information on traumatic bone bruising and marrow edema, and cinematic rendering generates lifelike images that give radiologists a direct view of injuries to surrounding ligaments and tendons. MRI is neither quick nor inexpensive, and often it’s not feasible to use in the acute period after major trauma.
“Patients might have hemodynamic instability that requires close monitoring in the ICU, or they might have life support equipment and orthopedic hardware that isn’t compatible with MRI,” Dr. Dreizin said. “CT is the routine workhorse for patients with known or suspected severe trauma, and the information from these post-processing techniques can serve as a stand-in when MRI isn’t in the cards.”
The team’s study included 54 patients with a mean age of 41 years, with instability grading for pelvic ring fractures by orthopedists using all available information from imaging, exam under anesthesia and clinical follow-up as the reference standard. The combined technique yielded significantly improved diagnostic performance, for discriminating stable, rotationally unstable and translationally (i.e., globally) unstable fractures, while agreement (weighted Kappa) between radiologists and the orthopedist reference standard improved from 0.44 to 0.76.
Additionally, the researchers discovered that, when examining specific anatomic areas, injuries to the sacroiliac joint, pubic symphysis, pelvic floor or iliolumbar ligaments increased the odds of instability 4- to 6-fold.
“We were also surprised to find that translational instability only occurred in patients with simultaneous disruption of all four major zones of injury,” Dr. Dreizin said. “Combined systematic evaluation of these regions with conventional CT images, dual-energy CT and cinematic rendering yielded 100% sensitivity for this severe form of instability in our sample.”
“CT is the routine workhorse for patients with known or suspected severe trauma, and the information from these post-processing techniques can serve as a stand-in when MRI isn’t in the cards.”
David Dreizin, MD
Technique Could Improve Diagnosis and Surgical Decision Making
Orthopedic surgeons are increasingly requesting conventional CT to supplement radiography for a variety of unstable injuries, and not just in the pelvis, noted Dr. Dreizin. Classification of traumatic injuries is still limited with CT, because the radiologist must infer the integrity of tendons and ligaments by the fracture pattern alone.
“Any technique that improves direct visualization of these structures or their bony attachments could make early grading more accurate and objective,” he said.
Dr. Dreizin added that the combined use of these techniques has many other potential applications—from the cervical spine to the extremities—that could ultimately improve diagnosis and surgical decision-making for patients with traumatic injuries.
For More Information
Access the Radiology study, “Dual-Energy CT and Cinematic Rendering to Improve Assessment of Pelvic Fracture Instability."
Read previous RSNA News articles about MSK radiology:
- Automating Hip Fracture Diagnosis with Deep Learning May Improve Recovery, Morbidity Rates
- Ultrasound Technique Predicts Hip Dysplasia in Infants