Novel Imaging Technique Accurately Assesses Cardiovascular Risks
Identifying plaque composition early can prevent life-threatening strokes

A new noninvasive technique for imaging the carotid artery offers advantages over other imaging methods and could provide an earlier, more accurate assessment of cardiovascular disease risk, according to a study in Radiology.
Imaging techniques like ultrasound (US), CT and MRI are useful for revealing the extent of narrowing in the carotid arteries, but are less helpful in determining the makeup of the plaque itself. This is a crucial limitation because plaque composition is associated with vulnerability to rupture, setting in motion the chain of events that leads to life-threatening strokes.
“Rapid characterization of tissue function and molecular composition is limited with these modalities, which commonly results in poor diagnostic accuracy and ineffective treatments,” said study senior author Daniel Razansky, PhD, director of the Functional and Molecular Imaging Lab at the University of Zurich and the Swiss Federal Institute of Technology in Zurich.
Dr. Razansky and colleagues studied volumetric multi-spectral optoacoustic tomography (vMSOT). As with US, vMSOT is performed with a handheld device that is moved against the neck. However, vMSOT employs spectroscopy to investigate tissue at a molecular scale. This provides information about the artery that is not attainable with other methods. It also can detect lipids, melanin and other disease-related biomarkers early enough to provide better treatment options.
“Unlike most other clinical imaging modalities mainly looking at late-stage anatomical manifestations of diseases, vMSOT is capable of sensing specific molecules in tissues without administration of contrast agents,” Dr. Razansky said. “In the case of carotid artery disease, assessment of the entire bifurcation area in real time and in 3D is only possible with vMSOT.”
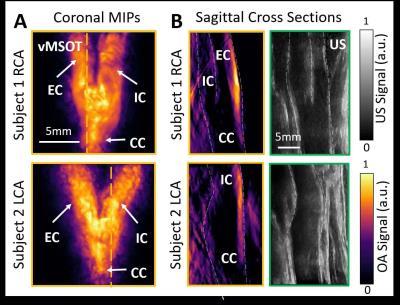
Images show qualitative comparison of image quality between volumetric multispectral optoacoustic tomographic (hereafter, vMSOT) and B-mode US in two volunteers. Right carotid artery (RCA) and left carotid artery (LCA) are shown in a 31-year-old woman (subject 1) and in a 26-year-old woman (subject 2), respectively. A, vMSOT images of carotid artery bifurcation in coronal view represented in maximum intensity projections (MIPs). B, vMSOT and B-mode US images of carotid bifurcation in sagittal cross-sectional views. Orange and green frames correspond to vMSOT and US images, respectively, where orange dashed lines in A indicate section shown in B. CC = common carotid, EC = external carotid, IC = internal carotid, OA = optoacoustic.
Technique Shows Potential for Clinical Use
The researchers performed vMSOT imaging on 16 healthy participants and compared results with those from conventional US. The vMSOT approach was able to noninvasively and instantaneously assess the entire bifurcation area of the carotid artery in three dimensions, making it less prone than US to motion-related, image-blurring artifacts. Results point to the tremendous potential of the new approach in the clinic.
“The developed handheld vMSOT imaging approach holds promise for rapid volumetric assessment of the carotid artery and plaque vulnerability in an entirely noninvasive manner,” Dr. Razansky said. “It also has the additional potential for label-free identification and assessment of clinically-relevant biomarkers of carotid artery disease, which helps with early and accurate diagnosis, timely treatment planning and monitoring.”
In the future, vMSOT could be combined with US for a more comprehensive characterization of the carotid artery.
“Given its fast imaging performance, excellent molecular contrast, portability and affordability, I truly believe that vMSOT will soon be routinely used in the clinic,” Dr. Razansky said. “One day, it may even become as popular as ultrasound.”
Web Extra
Access the Radiology study, “Real-time Volumetric Assessment of the Human Carotid Artery: Handheld Multispectral Optoacoustic Tomography,” at pubs.radiology.org.