New Research Shows PI-RADS Version 2 Effective in Prostate Cancer Diagnosis
Multiparametric MRI, with an interpretation using PI-RADS, can be very beneficial to the diagnosis of patients with prostate cancer.




While researchers have been studying MRI of the prostate for decades, it has only been in the last 10 years that multiparametric (mp) MRI has emerged as an effective tool to detect prostate cancer in men with raised serum PSA levels.
In 2012 the European Society of Urogenital Radiology (ESUR) published the Prostate Imaging Reporting and Data System (PI-RADS) — which included a scoring system — with the objective of standardizing the acquisition, interpretation and reporting of prostate MRI for cancer detection.
Clinical trials showed that PI-RADS v1 was able to improve the diagnosis of intermediate- to high-grade cancers compared to the standard of care TRUS biopsies. However, experience also showed that there were limitations associated with v1, and the American College of Radiology (ACR), ESUR and the AdMeTech Foundation established a steering committee to update and improve PI-RADS. The result was the development of PI-RADS version 2 (v2), which was introduced at RSNA 2014 and subsquently published in 2016. Since then, researchers worldwide have been working to validate PI-RADS v2.
In a recent 2018 online study in European Urology, members of the PI-RADS Steering Committee concluded that the evidence — from validation studies, systematic reviews and professional guidelines for mpMRI — shows that PI-RADS v2 retains higher accuracy over systematic transrectal ultrasound (TRUS) biopsies for prostate cancer diagnosis. And while PI-RADS v2 does not detect all cancers, it does detect the majority of tumors that can be harmful to patients.
“When you perform an mpMRI, with the interpretation using PI-RADS — and it is done well — it is very beneficial to the diagnosis of the patient and the therapeutic process,” said Jelle O. Barentsz, MD, PhD, a professor of radiology and chair of the Radboud Prostate MR-Reference Center of Radboud University Medical Center, the Netherlands, senior author of the European Urology article.
Radiology Study Focuses on Prostate Transition Zone
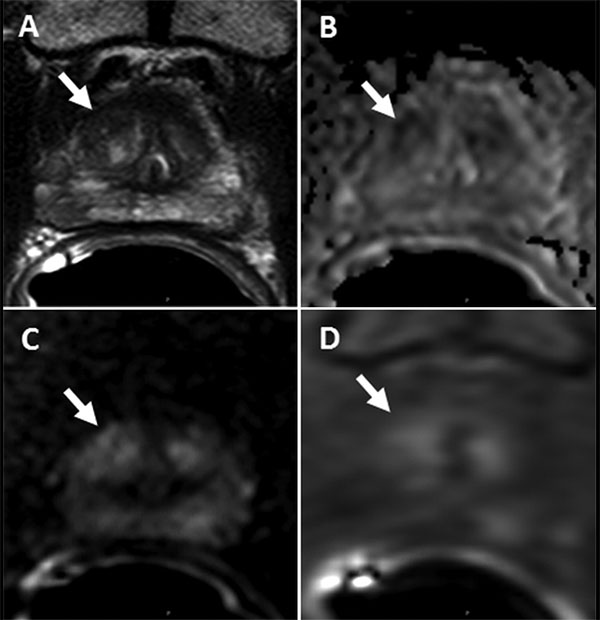
In an August 2018 Radiology study, author Peter Choyke, MD, and colleagues sought to determine the association between PI-RADS v2 scores and prostate cancer in patients undergoing biopsy of lesions in the prostate transition zone.
The prostate transition zone — a less frequent site of cancer compared to the peripheral zone —surrounds a part of the urethra that passes through the prostate and is a very complex environment, said Dr. Choyke, program director, Molecular Imaging Program, Center for Cancer Research at the National Institutes of Health, Bethesda.
“The prostate transition zone is also prone to hyperplasia and hyperplastic nodules,” Dr. Choyke said. “And the subcommittee was very concerned about whether PI-RADS v2 would work as well in the transition zone as it was predicted to work in the peripheral zone. And it turns out it is a pretty good predictor.”
Specifically, Dr. Choyke and his colleagues found that higher PI-RADS v2 scores are associated with a higher proportion of clinically significant cancers in the transition zone.
In the study, the researchers identified 634 transition zone lesions in 457 patients from a prospectively maintained database of patients undergoing prostate MRI and determined the proportion of cancer detection for all cancers, as well as clinically significant cancers for each PI-RADS v2 category.
For PI-RADS category 3, 4 and 5 lesions, the overall proportion of cancers was 22.2 percent (78 of 352), 39.1 percent (43 of 110), and 87.8 percent (129 of 147), respectively. In addition, the proportion of clinically important cancers was 11.1 percent (39 of 352), 29.1 percent (32 of 110), and 77.6 percent (114 of 147), respectively.
“We targeted those higher category lesions and sampled them,” said senior author Baris Turkbey, MD, associate research physician of the Molecular Imaging Program at the National Cancer Institute. “Specifically, those PI-RADS Category 5 lesions, which have more clinically significant cancers.”
For PI-RADS Category 2 lesions, the overall proportion of cancers was just 4 percent.
“And none of these were clinically significant,” Dr. Turkbey said. “This implies that these lesions probably should not be biopsied.”
Higher Quality Standards, Training Necessary
In their European Urology study, the PI-RADS Committee noted that mpMRI and MRI-directed biopsies using PI-RADS improves the detection of prostate cancers likely to cause harm, while decreasing the detection of those that will not.
“Nevertheless, the keys to success are high-quality imaging, reporting and biopsies by radiologists and urologists working together in multidisciplinary teams,” Dr. Barentsz said.
That means higher quality standards are needed in the both performing and interpreting prostate MRI scans, Dr. Barentsz said.
“And that quality assurance has to be everything in the diagnostic process, including the machines, the components of the scan, the readings and how that information gets communicated to urologists,” said lead author Anwar Padhani, MBBS, head of imaging research at the Paul Strickland Scanner Centre, Mount Vernon Cancer Center, London.
Dr. Barentsz said the biggest concern is the quality of the diffusion-weighted images. Because mpMRI is a relatively new modality, many radiologists were not exposed to it during their residency and fellowship training. Training is necessary, he said.
“Not every radiologist knows how to use PI-RADS,” Dr. Barentsz said. “Which is probably why courses on prostate MRI at RSNA are so popular. Many radiologists want to learn from the experts how to make the images and how to read them.”
Dr. Barentsz has organized a popular hands-on prostate MRI course at RSNA for several years and will offer it again at RSNA 2018.