Identifying Stroke Patients Likely to Benefit from IAT
Radiology research focuses on venous outflow as marker for patient's circulation


Recent studies have demonstrated the effectiveness of intraarterial therapy (IAT) on patients who have suffered an acute ischemic stroke if administered within six hours after the stroke.
However, while most patients benefit from IAT, those same studies showed that others did not fare well in terms of functional recovery after treatment, leaving researchers with questions about the best way to select patients who will actually benefit from the procedure.
In a recent study published in Radiology, Ivo G.H. Jansen, MD, Department of Radiology, Academic Medical Center, University of Amsterdam, the Netherlands, and colleagues determined that by assessing the level of cortical vein opacification in stroke patients through the use of CT angiography (CTA), they could determine which patients would or would not benefit from IAT.
While there are many patient characteristics — such as cerebral collateral flow — that may help physicians select patients who will benefit from IAT, none have been confirmed as a reliable, Dr. Jansen said. And that creates a problem considering the potential effectiveness of IAT, he added.
“So if you want to exclude someone from this treatment because you do not expect him or her to benefit, you want to be really certain,” Dr. Jansen said. “This means that research on these patient characteristics must be fairly robust before we can reliably tell someone – or someone’s family – that we will not be able to use IAT.”
Research Focuses on Three Veins
While research has primarily focused on such patient characteristics as collateral status and ischemic changes, the venous system has been relatively overlooked, Dr. Jansen said.
In their research, Dr. Jansen and senior author, Renė van den Berg, MD, PhD, Department of Radiology, Academic Medical Center, University of Amsterdam, hypothesized that venous outflow — as indicated on CTA — could be a marker for determining how well a patient’s circulation is working.
“We thought that if the blood is going through the tissue and coming out, the tissue must be functioning in some way — or least the microcirculation is functioning,” Dr. Jansen said. "This would indicate that the patient had less damage."
But if venous drainage is totally absent in the hemisphere in which the occlusion is located, we theorized that the microcirculation is damaged in some way so that blood is going in, but not coming out. So we started thinking about how to grade this.”
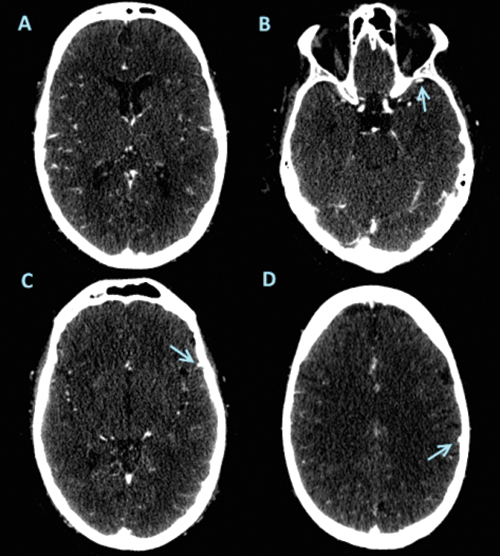
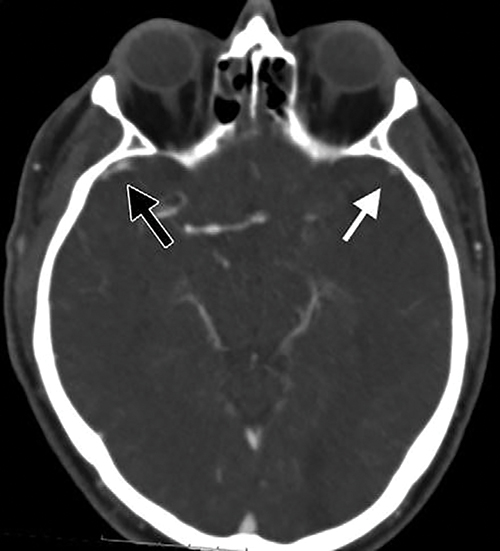
With the idea of determining levels of venous drainage that are markers for severe damage, Dr. Jansen and colleagues chose to examine three veins (the superficial middle cerebral vein, the vein of Labbe, and the sphenoparietal sinus) that are primarily responsible for draining the territory surrounding the middle cerebral artery — the area most commonly affected by massive strokes.
Their study was based on the dataset taken from the Multicenter Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN) held between 2000 and 2014. From that database, Dr. Jansen and colleagues retrospectively analyzed patients with baseline CT angiograms.
“We looked at each of the three veins individually,” Dr. Jansen said. “We looked at their opacification compared to the contralateral hemisphere and assessed whether there was no, moderate or full opacification of the vein.
Each of the veins was graded by a neurologist on a 0- to 2-point scale (0 = not visible, 1 = moderate opacification, and 2 = full opacification). A total sum was then calculated, which resulted in a cortical vein opacification score (COVES) ranging from 0 to 6.
The researchers found that patients with a COVES score of 0 — no opacification in any of the three veins — gained no benefit from IAT, while patients with a venous opacification (COVES score > 0) did benefit from the procedure.
Specifically, Dr. Jansen and his colleagues determined that in patients with a COVES score of 0 there was no shift toward a better functional outcome (adjusted common odds ratio: 1.0; 95 percent confidence interval (CI)) compared to a larger shift in patients with a COVES score greater than 0 (adjusted common odds ratio: 2.2; 95 percent CI).
Additionally, they found that mortality rates in patients with a COVES score of 0 at 7 and 30 days (18.7 percent and 26 percent respectively) were higher than those in patients with a COVES score greater than 0 (5.8 percent and 13.4 percent respectively).
“The results were pretty clear cut and what we expected,” Dr. Jansen said. “Findings indicated that if a person has a severely damaged brain due to stroke, the venous drainage will also be impacted and it can be assessed in the way we proposed.”
More Research Needed Before Clinical Use
In terms of using this patient selection method in the clinic, Dr. Jansen said more research is needed to confirm the results of this study. He added that using one particular parameter for patient selection for IAT may not be the best option.
“I think a combination of factors is the way to go here,” he said. “Maybe a combination of a collateral grade with a COVES score can add to the prognostic value of both parameters and give a more complete picture of what is going on with cerebral vasculature during a stroke.”
Web Extras
- Access the Radiology study, “Absence of Cortical Vein Opacification Is Associated with Lack of Intra-arterial Therapy Benefit in Stroke,” at https://pubs.rsna.org/doi/full/10.1148/radiol.2017162445