Study Suggests Intracranial Pathology Not Necessary for Gadolinium Deposition in Brain Tissues

Some research has suggested that minute traces of gadolinium are often retained in the brain tissue of patients years after undergoing MRI. But new Radiology research suggests that gadolinium retention may be more widespread and may be present in many more, or possibly all, patients exposed to gadolinium-based contrast agents.
“It’s estimated that approximately 400 million doses of gadolinium have been administered since 1988,” said the study’s lead researcher, Robert J. McDonald, MD, PhD, staff neuroradiologist at the Mayo Clinic in Rochester, MN. “Gadolinium contrast material is used in 40 to 50 percent of MRI scans performed today.”
Scientists previously believed gadolinium contrast material could not cross an intact blood brain barrier.
“By late 2014, the first evidence emerged that gadolinium was depositing within brain tissues. However, many of these patients had underlying medical conditions, such as brain tumors, that could adversely affect the blood brain barrier,” Dr. McDonald said. “We were curious if this deposition might be related to the integrity of the blood brain barrier, so we studied patients with normal brain pathology and presumably an intact blood brain barrier.”
The study involved an analysis of post-mortem neuronal tissue samples from five patients who had undergone four or more (up to 18) gadolinium-enhanced MRI exams between 2005 and 2015, and 10 patients who had undergone MRI exams without gadolinium. The median age at the time of death was 68 years in the contrast agent-exposed group and 79 years in the control group. All patients in the current study were exposed to gadodiamide (Omniscan).
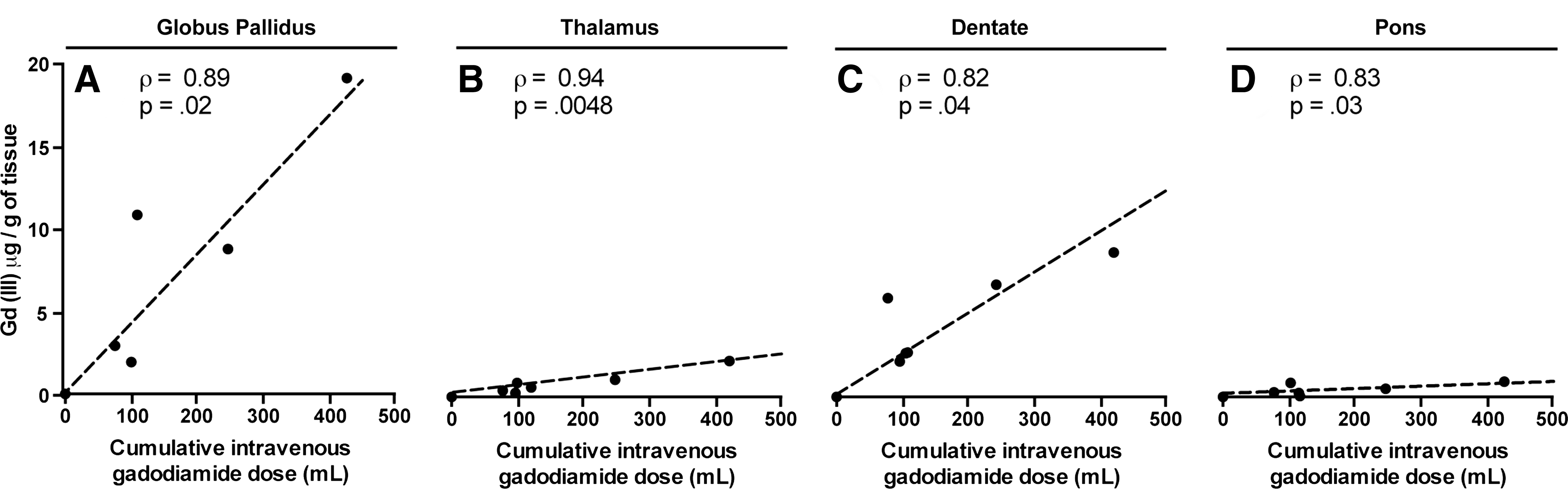
During the patient autopsies, a small amount of brain tissue was obtained from each patient and studied with transmission electron microscopy, mass spectroscopy and x-ray spectroscopy. The analysis revealed dose-dependent gadolinium deposits in four neuroanatomical regions of the brain in patients who underwent contrast-enhanced MRI. At the time of autopsy, all study patients had normal brain pathology.
“Our results suggest current thinking with regard to the permeability of the blood brain barrier is greatly oversimplified, as gadolinium appears to accumulate even among patients with normal brain tissue and no history of intracranial pathology,” Dr. McDonald said. “It will take additional research to understand how and why this deposition is occurring.”
The analysis revealed that certain areas of the brain, including the globus pallidus and dentate nucleus, retained more of the gadolinium agent. Because free gadolinium is similar to calcium in size and charge, Dr. McDonald said, the body may also mistake the contrast media for this endogenous metal, which is often taken up in areas of the brain during the aging process.
Despite finding evidence of gadolinium contrast agent deposition in the neural tissues, the researchers detected no histologic changes to suggest toxicity. The FDA has identified no convincing scientific evidence to date that these deposits are harmful, but is further investigating this matter.
“Gadolinium-based contrast agents have revolutionized MRI and diagnostic medicine,” Dr. McDonald said. “They have allowed us to detect diseases that would otherwise be extremely difficult to diagnose.”
Web Extras
- Access the Radiology study, “Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities,” at http://pubs.rsna.org/doi/full/10.1148/radiol.2017161595