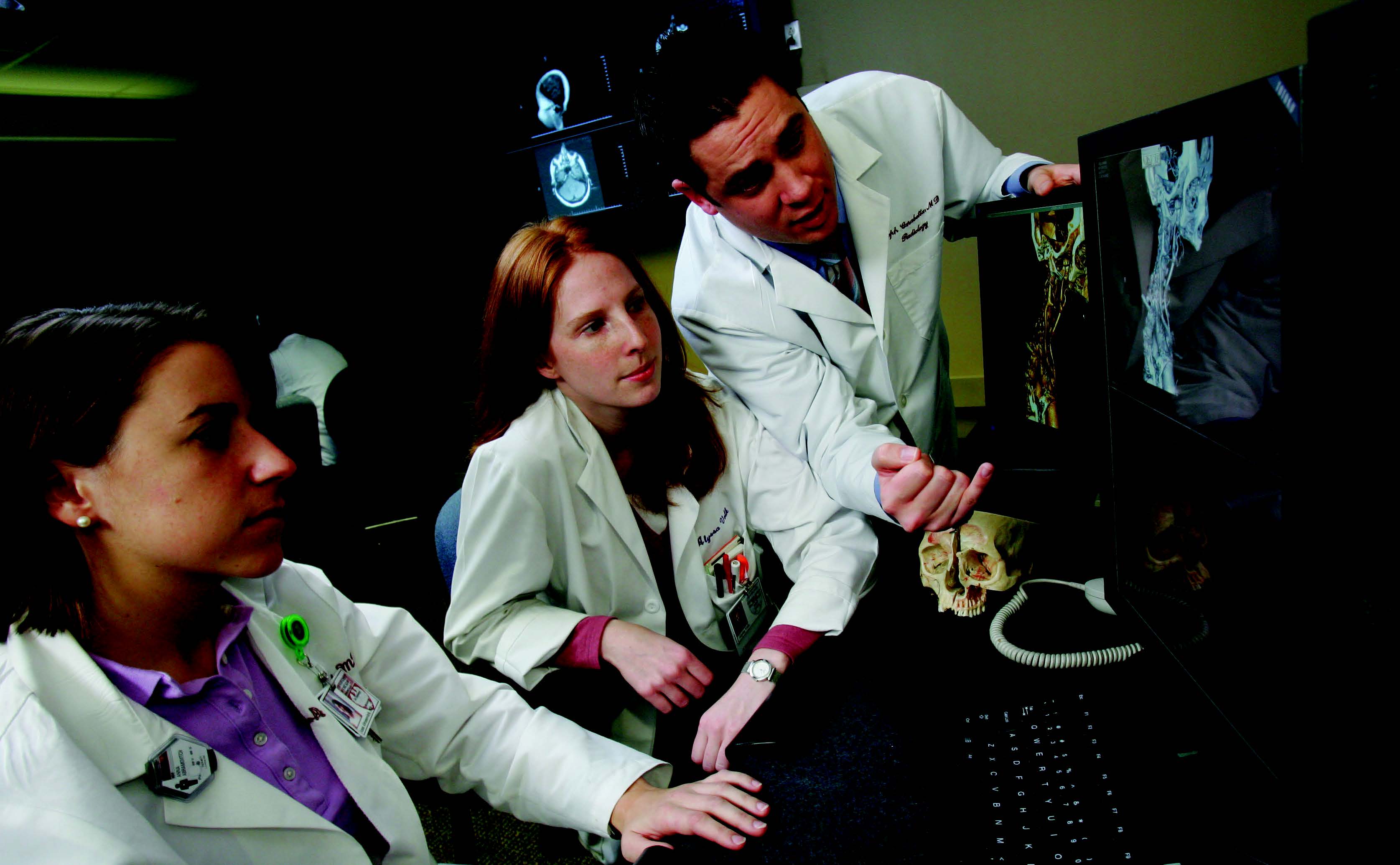
Radiologists, Referring Physicians Build Rapport with Patients
Cross-departmental collaboration is key to improving patient outcomes and engaging patients in the process



As the move toward patient-centered care intensifies, more healthcare facilities are realizing the value of cross-departmental collaboration in improving outcomes and engaging patients in their own healthcare. And imaging is occupying a front-row seat as more radiologists are meeting regularly not only with referring physicians, but also one-on-one with the patients in their care.
“Images are very powerful and allow us to enhance how we can communicate to our patients about their state of health,” said Garry Choy, M.D., M.B.A., a diagnostic radiologist at Massachusetts General Hospital (MGH), Boston.
In 2012, Dr. Choy and his colleagues launched a pilot program— the Radiology Consultation Clinic at MGH—in which patients who visit a primary care physician also review their images with a radiologist. While words convey a physician’s advice to stop smoking or embark on a diet and exercise program, images emphasize those messages. The hope is to halt or even reverse progression of diseases such as atherosclerosis and emphysema, Dr. Choy said.
“I like to tell the patients or joke around in a lighthearted way, ‘This is the ultimate selfie,’ ” he explained. “We’re looking inside your own body and your heart, and these are the plaques inside your coronary vessels.”
Since the pilot consultation clinic at MGH began, radiologists have been serving on the front lines as patient educators who advocate for better health, Dr. Choy said.
MGH Pilot Consultation Program Grows
The program originated when patients began asking to see their own images and speak with radiologists about terminology in reports. It began as one-on-one consultations based on requests from patients or referring physicians and mushroomed into a regularly scheduled clinic on Tuesdays embedded in primary care.
In the program, senior radiologists collaborate with Susan E. Bennett, M.D., a primary care physician at Internal Medicine Associates at MGH, to determine which patients on her schedule have undergone imaging scans revealing pathologic processes that may improve with lifestyle modification.
Dr. Bennett then offers these patients an opportunity to meet with a radiologist and discuss their results. “Usually, they say, ‘yes,’ they’re interested,”Dr. Bennett said. “We ask them ahead of time, ‘Do you know what a radiologist does? How would you feel about having a radiologist inform you about the results of your imaging examination? Afterwards, we ask them how they experienced the consultation.”
The program has been remarkably well-received. “With rare exception, patients have really been pleased to view their images with a radiologist,” Dr. Bennett said. For most patients, it is the first time that a radiologist has shared images with them as opposed to forwarding the findings to the ordering physician.
Seeing the images enlightens patients in a number of ways. They are able to visualize findings such as coronary artery calcification, fatty infiltration of the liver and mild centrilobular emphysema that could develop into a more severe form. Or they may be reassured that a small nodule is not posing any immediate danger.
To establish benchmarks, the program measures satisfaction on the part of patients and referring physicians, as well as patient engagement in their own care. “In this field, there are emerging metrics in value-based care,” Dr. Choy said. “We, as radiologists, can now also play a role.”
A Paradigm Shift for Radiology
As medicine moves toward patient-centered radiology, programs similar to the one at MGH are of increasingly significant value, said Judy Yee, M.D., vice-chair of radiology and biomedical imaging at the University of California San Francisco, past-chair of the RSNA Public Information Committee (PIC) and a member of the RSNA Public Information Advisors Network (PIAN).
“It takes the radiologist out of this black box and puts him or her front and center as a physician who is invested in taking care of patients,” Dr. Yee said. “It’s a different paradigm, and it’s a bit of a culture change for radiologists.”
Allocating time and funding for these consultations can be challenging, but in competitive markets, it helps physicians build rapport with patients. Based on patients’ experiences with mammography and interventional radiology, they tend to appreciate personalized interaction with radiologists, said Dr. Yee, also chief of radiology at San Francisco VA Medical Center.
Although Dr. Bennett has convenient access to radiologists at MGH, primary care physicians located in separate facilities or cities could offer patients virtual consultations with radiologists via video conferencing, she said.
“It’s key that physicians understand that patients really like this,” Dr. Bennett said. “At the end of the day, it’s not what we feel comfortable with; it’s what works best for patients.”\
Discussing the importance of the role between radiologists and referring physicians in patient care
Web Extras
Access RSNA’s full roster of resources to optimize the patient experience, including:
- RadiologyInfo.org, the public information resource developed by RSNA and the American College of Radiology (ACR), offers information on more than 200 radiologic procedures with easy-to-understand descriptions about what to expect during imaging exams, how to prepare and more. It also includes information about diseases and conditions, as well as articles about wellness screening.

- Radiology Cares® (RSNA.org/Radiology_Cares) offers resources and educational materials to help radiology professionals take patient-centered radiology from concept to practice, from scheduling through follow-up communications to better align their practices with their patients’ needs.
